Medical Books Free for Doctors
Are You searching for any Medical Books? Please post the name on the wall. We will try to provide You the Free download link.Please share this page.Invite Your Friend to join here to get all types of Free Medical Books.

Search Here

Custom Search
Showing posts with label Anatomy. Show all posts
Showing posts with label Anatomy. Show all posts
Tuesday, November 20, 2012
Tuesday, December 27, 2011
Triangle of Auscultation

The triangle of ausculation of the lungs is situated posterior and superficial to the scapula.
It has the following boundaries:
- Superiorly, by the Trapezius
- Inferiorly, by the Latissimus dorsi
- Laterally by the medial margin of the scapula
The floor is partly formed by the Rhomboideus major and parts of 6th and 7th ribs.
The triangle of auscultation is a space on the back where the relatively thin musculature allows for respiratory sounds to be heard more clearly with a stethoscope.
To better expose the floor of the triangle, which is made up of the posterior thoracic wall in the 6th intercostal space, the patient is asked to fold their arms across their chest, medially rotating the scapulae, while bending forward at the trunk.
 Posted in: Anatomy
Posted in: AnatomyFEMORAL TRIANGLE
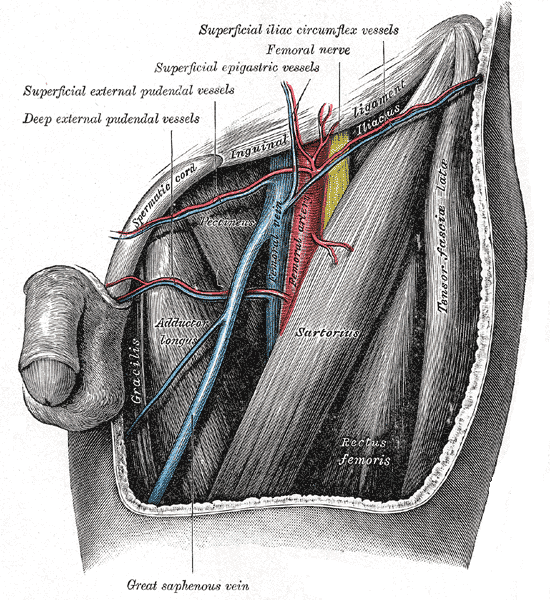

BOUNDARIES OF FEMORAL CANAL :
Bounded by:
- (superiorly) the inguinal ligament
- (medially) the medial border of the adductor longus muscle
- (laterally) medial border of the sartorius muscle
- Its floor is provided laterally by iliopsoas, medially by pectineus and adductor longus. Its roof is formed by the fascia lata.
- The femoral triangle is shaped like the sail of a ship.
- Its boundaries can be remembered using the mnemonic, "SAIL" for Sartorius, Adductor longus and Inguinal Ligament.
CONTENTS :
It is important as a number of vital structures pass through it, right under the skin.
The following structures are contained within the femoral triangle (from lateral to medial):
- terminal part of the femoral nerve and its branches
- femoral sheath
- femoral artery and its branches
- femoral veins and its tributaries
- femoral canal, containing the deep inguinal lymph nodes (snell, 8th edition)
- FLOOR
- iliopsoas
- pectineus
- adductor longus
- Lacunar Ligament
- ROOF is formed by the skin and fascia lata.
CLINICAL SIGNIFICANCE:
Since the femoral triangle provides easy access to a major artery, coronary angioplasty and peripheral angioplasty is often performed by entering the femoral artery at the femoral triangle. Heavy bleeding in the leg can be stopped by applying pressure to points in the femoral triangle. Another clinical significance of the femoral triangle is that the femoral artery is positioned at the midinguinal point (midpoint between the pubic symphysis and the anterior superior iliac spine); medial to it lies the femoral vein. Thus the femoral vein, once located, allows for femoral venopuncture[citation needed]. Femoral venopuncture is useful when there are no superficial veins that can be aspirated in a patient, in the case of collapse.
The positive pulsation of the femoral artery signifies that the heart is beating and also blood is flowing to the lower extremity[citation needed].It is also necessary to appreciate clinically that this is a case where the nerve is more lateral than the vein. In most other cases the a nerve (relative to its associated artery and vein)would be the deepest or more medial followed by the artery and then the vein. But in this case it is the opposite. This must be remembered when venous or arterial samples are required from the femoral vessels. The order of this neurovascular bundle can be remembered using the mnemonic, "NAVY" for Nerve, Artery, Vein, Y -fronts (the British term of a style of men's underwear with a "Y" shaped front that acts as a fly). The "Y" is midline (corresponding with the penis) and the mnemonic always reads from the outside - in, so that the Femoral Nerve is always lateral. An alternate to this mnemonic is "NAVaL" for Nerve, Artery, Vein, and Lymph, to include the deep inguinal lymph nodes located medial to the Femoral vein.
 Posted in: Anatomy
Posted in: AnatomyCoronary arteries and Coronary veins
![[Coronary_arteries_and_veins1.jpg]](https://blogger.googleusercontent.com/img/b/R29vZ2xl/AVvXsEhNQuXFTvfS0VaK8EwYwhV9P_1OTvFDZWlRkcOoOjI6mMvZBmj-cVDdzhI4W23dZn1p_eGXgPhmJTc6doU_hbMKMLci2qtw2T2tEvjws57xGe6rF4mNQWR65JFTFLwvwzUpQXcZ1CYgWEI/s1600/Coronary_arteries_and_veins1.jpg)
![[Coronary_arteries_and_veins2.jpg]](https://blogger.googleusercontent.com/img/b/R29vZ2xl/AVvXsEj7qgO03BX3T5c8ONm0IQx1MlDuJxK2wsP91Wycwzsh73MEdTQD_zW-iOJTNqtykTH4QclsdjU4uz6g95hW4PM0KyOUe0nNXt-mAPanvVMpGBS7tNvMiBxAd_jtTQBFU6mZh9jHsGl_MjY/s1600/Coronary_arteries_and_veins2.jpg)
The coronary arteries and the veins that drain into the coronary sinus. The posterior interventricular branch (PIV), although usually a branch of the right coronary artery (RC), may arise from the circumflex branch (C) of the left coronary artery (inset). In B, the left marginal vein can be seen ascending to join the great cardiac vein. The posterior vein of the left ventricle ascends and the oblique vein of the left atrium descends to end in the coronary sinus.
AIV, anterior interventricular branch; C, circumflex branch; GC, great cardiac vein; LC, left coronary artery; MC, middle cardiac vein; PIV, posterior interventricular branch; Re, right coronary artery; S.-A, branch to sinuatrial node; SC, small cardiac vein.
AIV, anterior interventricular branch; C, circumflex branch; GC, great cardiac vein; LC, left coronary artery; MC, middle cardiac vein; PIV, posterior interventricular branch; Re, right coronary artery; S.-A, branch to sinuatrial node; SC, small cardiac vein.
 Posted in: Anatomy
Posted in: AnatomyAnatomical Snuff Box
![[anatomical_snuff_box.JPG]](https://blogger.googleusercontent.com/img/b/R29vZ2xl/AVvXsEjDcVWUucI4EDLKx3suAjv-_-QLbllhTk6IZD79qCEr2CoNWaw4EZGdPK7qlb8dzZpEgawweZ1zQQqsfibzWyyIAtBYTyHXZaKmg1GS0OlWqyuxC0a8-EJZ5_inau1_lsGOiRGqOpbPgBM/s1600/anatomical_snuff_box.JPG)
Anatomical snuff box is a triangular depression on the lateral aspect of wrist immediately distal to the radial styloid process, that becomes prominent when thumb is fully extended.
The Contents of anatomical snuff box are :
- Cephalic vein
- Radial artery
- Superficial radial nerve
Floor of the anatomical snuff box is formed by :
- Radial styloid
- Scaphoid (smooth convex articular surface)
- Trapezium
- Base of First metacarpal
BOUNDARIES OF ANATOMICAL SNUFF BOX :
Lateral/Anterior wall
- Abductor Pollicis Longus (Radially)
- Extensor Pollicis Brevis (Medially)
- Extensor Pollicis Longus
 Posted in: Anatomy
Posted in: AnatomyMedial and Lateral Menisci of Knee joint
![[medial_lateral_meniscus.jpg]](https://blogger.googleusercontent.com/img/b/R29vZ2xl/AVvXsEiFmTYgnc2Kj5KERWn1OE0ETvYc4YzA8sgQ61rKaEsaKZEiD0iRqGTplMlHmnc_cwaz60_rsHB4CjHreJw54u45y0wlNMradWBedahl8ZjFf5EBRT_bZrw54Q8HKP_UfEi8wWCna2K5BdI/s1600/medial_lateral_meniscus.jpg)
The menisci of the knee joint are two pads of cartilaginous tissue which serve to disperse friction in the knee joint between the lower leg (tibia) and the thigh (femur). They are shaped concave on the top and flat on the bottom, articulating with the tibia. They are attached to the small depressions (fossae) between the condyles of the tibia (intercondyloid fossa), and towards the center they are unattached and their shape narrows to a thin shelf.
Both are cartilaginous tissues that provide structural integrity to the knee when it undergoes tension and torsion. The menisci are also known as 'semi-lunar' cartilages — referring to their half-moon "C" shape — a term which has been largely dropped by the medical profession, but which led to the menisci being called knee 'cartilages' by the lay public.
The menisci act to disperse the weight of the body and reduce friction during movement. Since the condyles of the femur and tibia meet at one point (which changes during flexion and extension), the menisci spread the load of the body's weight. This differs from sesamoid bones, which are made of osseous tissue and whose function primarily is to protect the nearby tendon and to increase its mechanical effect.
SUMMARY:
Both the Medial and lateral menisci are outside the synovial cavity but within the joint cavity.
The Medial meniscus is larger than the lateral meniscus.
The Medial meniscus is C shaped where as the lateral mensicus is circular shaped.
The Medial meniscus is directly attached to the medial collateral ligament, where as the Popliteal muscle interferes in between the attachment of lateral meniscus and lateral collateral ligament.
The Medial collateral ligament is most commonly injured when compared with the lateral collateral ligament.
 Posted in: Anatomy
Posted in: AnatomyLymph nodes of Neck

The lymph nodes of the neck can be divided into six levels within the defined anatomic triangles. These groups and the areas that they drain are particularly important when locating and working up a "neck mass" or possible malignancy.
The groups and drainage areas are as follows:
- I--Submental and submandibular nodes
- II--Upper jugulodigastric group
- III--Middle jugular nodes (draining the nasopharynx and oropharynx, oral cavity, hypopharynx, larynx.
- IV--Inferior jugular nodes draining the hypopharynx, subglottic larynx, thyroid, and esophagus.
- V-- Posterior triangle group
- VI--Anterior compartment group
Adductor canal (Subsartorial/Hunter's canal)
![[Adductor_canal.png]](https://blogger.googleusercontent.com/img/b/R29vZ2xl/AVvXsEhmQM8aTm8zwfWXbayVIMK65U21XPpglKJI2q32crsCj1sYP9ELKm_5kw2Uq-JHXroA4rsIXxc6DMaldelyrzzOiHJaxJyn78xVdMrR9deV_9WluZ9-650VNaWteqMO5FT4C_K754el0Tc/s1600/Adductor_canal.png)
The adductor canal (Subsartorial/Hunter’s canal) is an aponeurotic tunnel in the middle third of the thigh, extending from the apex of the femoral triangle to the opening in the Adductor magnus, the Adductor hiatus.
It courses between the anterior compartment of thigh and the medial compartment of thigh, and has the following boundaries:
- Anterolaterally - the Vastus medialis.
- Posterior - the Adductor longus. It is covered in by a strong aponeurosis which extends from the Vastus medialis, across the femoral vessels to the Adductor longus and magnus.
Lying on the aponeurosis is the Sartorius muscle.
The canal contains the femoral artery, femoral vein, and branches of the femoral nerve (specifically, the saphenous nerve, and the nerve to the Vastus medialis).
Named after JOHN HUNTER.
 Posted in: Anatomy
Posted in: AnatomyUterine artery

- The uterine artery arises from the anterior trunk of the internal iliac artery(hypogastric artery) .
- Its course is at first downwards and forwards until it reaches the parametrium when it turns medially towards the uterus.
- It reaches the uterus at the level of the internal os, where it turns upwards, at right angles, and follows a spiral course along the lateral border of the uterus to the region of the uterine cornu.
- Here it sends a branch to supply the fallopian tube and ends by anastomosing with the ovarian artery.
- The tortuosity is lost when the uterus enlarges during pregnancy.
- During the vertical part of its course it sends branches which run transversely and pass into the myometrium.
These are called the arcuate arteries.
- From these arcuate arteries, a series of radial arteries arise, almost at right angles.
- These radial arteries reach the basal layers of the endometrium, where they are termed as the basal arteries.
- From these are derived the terminal spiral and straight arterioles of the endometrium.
- THE LEAST VASCULAR PART OF THE UTERUS IS THE MIDLINE.
The branches of the uterine artery are :
- Ureteric artery
- Descending vaginal artery- These unite to form the anterior and posterior azygos artery of the vagina. This is of great importance during the Total hysterectomy.
- Circular cervical
- Arcuate -- radial -- basal -- spiral and straight arterioles of the functional layer of the endometrium.Anastomotic branch with the ovarian artery
- The relation of the uterine artery to the ureter is of great importance.
- The uterine artery crosses above the ureter in the parametrium where it gives off an important ureteric branch to that structure.
- The artery runs transversely while the ureter runs approximately anteroposteriorly through the ureteric canal of the parametrium.
The ovarian artery is derived from the AORTA.
Pelvic diaphragm
![[pelvic-diaphragm.jpg]](https://blogger.googleusercontent.com/img/b/R29vZ2xl/AVvXsEjXWnH3jMTEMPzvH6-WVrPK6pWTd8OuHirpaxcKDIdjrdzuQectA_J4Mr4QBuGz8dAk8BpsgYM2GODixvAzAh1DcSkuU4dc-2kFHrKf2q4d_Arl1yVv49LcXfDOvIbSmXFWRz3YQsYfTkE/s1600/pelvic-diaphragm.jpg)
The pelvic floor or pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus(ishciococcygeus), and associated connective tissue which span the area underneath the pelvis. The pelvic diaphragm is a muscular partition formed by the levatores ani and coccygei, with which may be included the parietal pelvic fascia on their upper and lower aspects. The pelvic floor separates the pelvic cavity above from the perineal region (including perineum) below.
The right and left levator ani lie almost horizontally in the floor of the pelvis, separated by a narrow gap that transmits the urethra, vagina, and anal canal. The levator ani is usually considered in three parts: pubococcygeus, puborectalis, and iliococcygeus. The pubococcygeus, the main part of the levator, runs backward from the body of the pubis toward the coccyx and may be damaged during parturition. Some fibers are inserted into the prostate, urethra, and vagina. The right and left puborectalis unite behind the anorectal junction to form a muscular sling . Some regard them as a part of the sphincter ani externus. The iliococcygeus, the most posterior part of the levator ani, is often poorly developed.
The coccygeus(ischiococcygeus), situated behind the levator ani and frequently tendinous as much as muscular, extends from the ischial spine to the lateral margin of the sacrum and coccyx.
The pelvic cavity of the true pelvis has the pelvic floor as its inferior border (and the pelvic brim as its superior border.) The perineum has the pelvic floor as its superior border.
Some sources do not consider "pelvic floor" and "pelvic diaphragm" to be identical, with the "diaphragm" consisting of only the levator ani and coccygeus, while the "floor" also includes the perineal membrane and deep perineal pouch. However, other sources include the fascia as part of the diaphragm. In practice, the two terms are often used interchangeably.
Inferiorly, the pelvic floor extends into the anal triangle.
Video :
 Posted in: Anatomy
Posted in: AnatomyUrogenital diaphragm
Most of the support of the perineum is provided by the pelvic and urogenital diaphragms.
The urogenital diaphragm is external to the pelvic diaphragm and includes the triangular area between the ischial tuberosities and the symphysis. The urogenital diaphragm is made up of the deep transverse perineal muscles, the constrictor of the urethra, and the internal and external fascial coverings (perineal membrane).

The urogenital diaphragm is external to the pelvic diaphragm and includes the triangular area between the ischial tuberosities and the symphysis. The urogenital diaphragm is made up of the deep transverse perineal muscles, the constrictor of the urethra, and the internal and external fascial coverings (perineal membrane).

Video:
Perineal body
The perineal body (or central tendon of perineum) is a pyramidal fibromuscular mass in the middle line of the perineum at the junction between the urogenital triangle and the anal triangle . It is found in both males and females. In males, it is found between the bulb of penis and the anus; in females, is found between the vagina and anus, and about 1.25 cm in front of the latter.
The perineal body is essential for the integrity of the pelvic floor, particularly in females. Its rupture during delivery leads to widening of the gap between the anterior free borders of levator ani muscle of both sides, thus predisposing the woman to prolapse of the uterus, rectum, or even the urinary bladder.
At this point, the following muscles converge and are attached:

The perineal body is essential for the integrity of the pelvic floor, particularly in females. Its rupture during delivery leads to widening of the gap between the anterior free borders of levator ani muscle of both sides, thus predisposing the woman to prolapse of the uterus, rectum, or even the urinary bladder.
At this point, the following muscles converge and are attached:
- External anal sphincter
- Fibers from external urinary sphincter
- Superficial transverse perineal muscle
- Deep transverse perineal muscle
- Anterior fibers of the levator ani
- Bulbospongiosus

Muscles of Perineum/Urogenital region


SUPERFICIAL MUSCLES OF PERINEUM :
- Superficial Transverse perinei
- Bulbospongiosus (Bulbocavernosus in older textbooks)
- Ischiocavernosus
DEEP MUSCLES OF PERINEUM :
- Deep Transverse Perinei
- Sphincter urethrae
 Posted in: Anatomy
Posted in: AnatomySkull Foramina

2. Palatine Process of Maxilla
3. Palatine
4. Greater Palatine Foramen
5. Lesser Palatine Foramen
6. Pterygoid Processes of Sphenoid
7. Zygomatic Process
8. Squamous Part of Temporal Bone
9. Mandibular Fossa
10. Styloid Process
11. Stylomastoid Foramen
12. Mastoid Process
13. Mastoid Foramen
14. Superior Nuchal Line
15. External Occipital Protruberance
16. Median Nuchal Line
17. Inferior Nuchal Line
18. Foramen Magnum
19. Condyloid Canal
20. Occipital Condyle
21. Hypoglossal Canal
22. Jugular Foramen
23. Carotid Canal
24. Foramen Spinosum
25. Foramen Ovale
26. Foramen Lacerum
27. Vomer
28. Transverse Palatine Suture
29. Median Palatine Suture
 Posted in: Anatomy
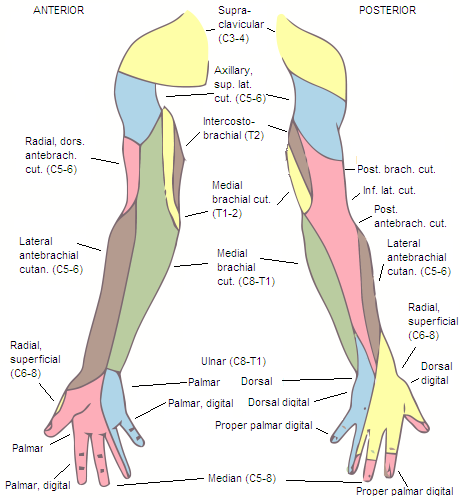
Posted in: AnatomyMusculocutaneous nerve


PATH OF THE NERVE :
The musculocutaneous nerve arises from the lateral cord of the brachial plexus, opposite the lower border of the Pectoralis minor, its fibers being derived from C5, C6, C7.
It penetrates the Coracobrachialis muscle and passes obliquely between the Biceps brachii and the Brachialis, to the lateral side of the arm; a little above the elbow it pierces the deep fascia lateral to the tendon of the Biceps brachii and is continued into the forearm as the lateral antebrachial cutaneous nerve.
In its course through the arm it innervates the Coracobrachialis, Biceps brachii, and the greater part of the Brachialis.
- The branch to the Coracobrachialis is given off from the nerve close to its origin, and in some instances as a separate filament from the lateral cord of the plexus; it is derived from the seventh, cervical nerve.
- The branches to the Biceps brachii and Brachialis are given off after the musculocutaneous has pierced the Coracobrachialis; that supplying the Brachialis gives a filament to the elbow-joint.
- The nerve also sends a small branch to the bone, which enters the nutrient foramen with the accompanying artery.
IRREGULARITIES :
The musculocutaneous nerve presents frequent irregularities.
It may adhere for some distance to the median and then pass outward, beneath the Biceps brachii, instead of through the Coracobrachialis.
Some of the fibers of the median may run for some distance in the musculocutaneous and then leave it to join their proper trunk; less frequently the reverse is the case, and the median sends a branch to join the musculocutaneous.
The nerve may pass under the Coracobrachialis or through the Biceps brachii.
Occasionally it gives a filament to the Pronator teres, and it supplies the dorsal surface of the thumb when the superficial branch of the radial nerve is absent.
DAMAGE :
Although rare, the musculocutaneous n. can be affected through compression due to hypertrophy or entrapment between the biceps aponeurosis & brachialis fascia or it may be injured through stretch as occurs in dislocations & sometimes in surgery.
Isolated injury, causes weakness of elbow flexion & supination of the forearm.
A discrete sensory disturbance is present on the radial side of the forearm.
The nerve is usually involved in an upper brachial plexus palsy
Injury can occur before entering the coracobrachialis due to dislocation or apparently due to stretch due to throwing injury
Heavy backpacks can cause damage to the upper trunk of the brachial plexus – dysfunction can be severe & prolonged with similar injury as occurs with Erb's palsy from breech deliveries. Early detection is important – the combination of time, avoidance of wearing a backpack, and strengthening of the shoulder muscles will probably be effective.
Distal to the coracobrachialis, the MC cause appears to be weight lifting – either through compression due to hypertrophy or entrapment between the biceps & brachialis, the nerve may lead to a painless loss of muscle strength in flexion & supination of the forearm. Initial treatment should include avoidance of biceps curls or other biceps exercises.
 Posted in: Anatomy
Posted in: Anatomy






 12:46 PM
12:46 PM
 T
T




![[pelvislateral.jpg]](https://blogger.googleusercontent.com/img/b/R29vZ2xl/AVvXsEjDAfQzJT0KCq50SAVjl44Cn9EFGGCD3TtYuRqR624Kyab61L9G-hp_Q_u_Q2_c4PT2-IQrNMrpjACcxVXhViRok8ky5t3QD8rXYfDe2jnHs4GMdpVbrtGPJg2cyjuUfoIKg30cnuZ8dKE/s1600/pelvislateral.jpg)
![[pelvisposterior.jpg]](https://blogger.googleusercontent.com/img/b/R29vZ2xl/AVvXsEjvwXFoAkLv2E6R9-zbh1SIY3BNxY-EtTV9YFiZv5ZqYnONPUhKL2hAYPDiE3yQF30NiyhXicZl73whpLryGYtoT_Q53qJn8o1kkE93k9_n0N_A1ZGcPNF6Y67w58uOWP3C6oBc8irhyho/s1600/pelvisposterior.jpg)







